Search
Research
Spatial codistribution of HIV, tuberculosis and malaria in EthiopiaHIV, tuberculosis (TB) and malaria are the three most important infectious diseases in Ethiopia, and sub-Saharan Africa. Understanding the spatial codistribution of these diseases is critical for designing geographically targeted and integrated disease control programmes. This study investigated the spatial overlap and drivers of HIV, TB and malaria prevalence in Ethiopia.
Research
Gaussian random fields: with and without covariancesWe begin with isotropic Gaussian random fields, and show how the Bochner-Godement theorem gives a natural way to describe their covariance structure. We continue with a study of Matérn processes on Euclidean space, spheres, manifolds and graphs, using Bessel potentials and stochastic partial differential equations (SPDEs).
News & Events
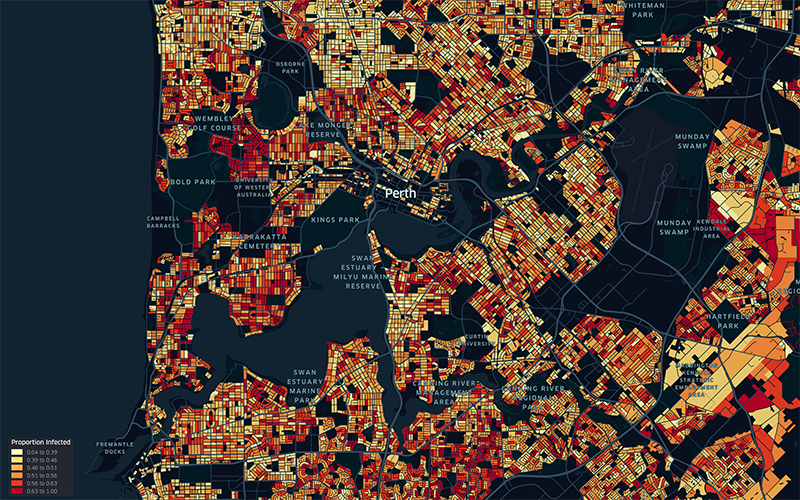
Sophisticated new modelling suggests keeping mask mandate could prevent 147,000 COVID-19 casesWA’s current Omicron COVID-19 outbreak could jump by 147,000 cases if mask mandates are abandoned before the Easter long weekend, according to sophisticated new modelling.

News & Events
New study identifies African ‘hotspot’ for highly infectious diseasesA regional corner of Africa is a hotspot for cases of HIV, tuberculosis and malaria, prompting researchers to call for targeted health support rather than a national response.
Research
Comparison of new computational methods for spatial modelling of malariaGeostatistical analysis of health data is increasingly used to model spatial variation in malaria prevalence, burden, and other metrics. Traditional inference methods for geostatistical modelling are notoriously computationally intensive, motivating the development of newer, approximate methods for geostatistical analysis or, more broadly, computational modelling of spatial processes.
Research
Trends in treatment-seeking for fever in children under five years old in 151 countries from 1990 to 2020Access to medical treatment for fever is essential to prevent morbidity and mortality in individuals and to prevent transmission of communicable febrile illness in communities. Quantification of the rates at which treatment is accessed is critical for health system planning and a prerequisite for disease burden estimates.
Research
Community knowledge, attitude, practices and beliefs associated with persistence of malaria transmission in North-western and Southern regions of TanzaniaDespite significant decline in the past two decades, malaria is still a major public health concern in Tanzania; with over 93% of the population still at risk. Community knowledge, attitudes and practices, and beliefs are key in enhancing uptake and utilization of malaria control interventions, but there is a lack of information on their contribution to effective control of the disease.
Research
Geospatial joint modeling of vector and parasite serology to microstratify malaria transmissionThe World Health Organization identifies a strong surveillance system for malaria and its mosquito vector as an essential pillar of the malaria elimination agenda. Anopheles salivary antibodies are emerging biomarkers of exposure to mosquito bites that potentially overcome sensitivity and logistical constraints of traditional entomological surveys.
Research
Malaria treatment for prevention: a modelling study of the impact of routine case management on malaria prevalence and burdenTesting and treating symptomatic malaria cases is crucial for case management, but it may also prevent future illness by reducing mean infection duration. Measuring the impact of effective treatment on burden and transmission via field studies or routine surveillance systems is difficult and potentially unethical. This project uses mathematical modeling to explore how increasing treatment of symptomatic cases impacts malaria prevalence and incidence.
Research
Human movement and environmental barriers shape the emergence of dengueUnderstanding how emerging infectious diseases spread within and between countries is essential to contain future pandemics. Spread to new areas requires connectivity between one or more sources and a suitable local environment, but how these two factors interact at different stages of disease emergence remains largely unknown.
